Disclosure :: This post is written by Dr. Anita Gouri of Lafayette Pediatric Dentistry. Tongue Ties are a large conversation in the community right now. If you want to read more about Tongue Ties (aka the truth about tongue and lip-ties) you can do so HERE.
Tongue Ties Part 2: Why a “Quick Snip” is Rarely a Quick Fix
 Whether it’s done with a laser or scissors, in the office or in the hospital, in infancy or adulthood, tongue tie releases (also known as tongue tie clipping or frenectomy), are rarely a quick fix.
Whether it’s done with a laser or scissors, in the office or in the hospital, in infancy or adulthood, tongue tie releases (also known as tongue tie clipping or frenectomy), are rarely a quick fix.
A quick review: a tongue tie (also known as a frenum or frenulum) is a band of tissue that attaches the underside of the tongue to the floor of the mouth. Everyone has a frenum, but many are too short, too thick, or attached too near the front of the mouth, which may cause restriction of proper tongue movement and therefore function. When this occurs, the frenum becomes a tongue tie, because literally the tongue is tied down to the floor of the mouth, when it should be resting against the roof of the mouth.
Why cutting a frenum is not a quick fix: A tongue tie acts like an anchor, limiting movement of the tongue. As a result, the extraoral (facial) muscles such as the lips and jaw muscles have to compensate for the lack of tongue movements. When the tongue tie is released, the facial muscles remain “programmed” to compensate, while the tongue continues to lack the muscle memory or strength to function properly. So, feeding difficulties often persist after the tongue tie is clipped. Only proper therapy after release can help correct this. This can be true even for newborns: a baby begins to use the tongue to swallow amniotic fluid as early as 20 weeks in utero. If they are tied, they are born with impaired tongue function.
Many insist that the tongue will “automatically” know to elevate towards the palate as soon as the tongue tie is clipped. We hope and pray that every baby falls into this category, but I’m here to tell you, that after treating literally hundreds of babies for tongue tie, this is rarely true. Too many times, I have patients come to my office for a second opinion who have had their tongue tie released as an infant, yet continue to have feeding, speech, and airway difficulties into toddlerhood. A quick inspection of their tongue’s resting position shows it still resting at the bottom of their mouth, as though the tongue tie was still present. Their facial muscles continue to function in a compensatory fashion.
Some examples of common compensations: With regards to feeding, we often find that the child cannot process foods that aren’t pureed or soft. It is often mislabeled as picky eating, but the truth is, because the tongue is inhibited from contacting the palate fully, the swallow pattern is inhibited from maturing to handle bulkier, more fibrous foods. So we often see the child begin to prefer only softer foods like rice and gravy, processed meats, and mashable produce, which can be processed with minimal tongue movement. Foods that are more textured or bulky, which require more tongue movement, are rejected because they cause gagging or a “choking” feeling while attempting to eat.
With sleep, I see adults who tell me they cannot fully recline without feelings of “choking” or shortness of breath: when the tongue doesn’t elevate towards the palate on its own, it 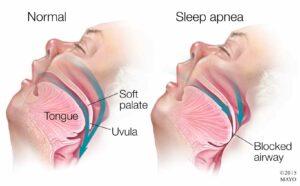 can fall back into the airway while sleeping. As a result they sleep only partially reclined. I once studied a patient who insisted on sucking their thumb at night, well into their middle school years, “because it’s the only way I can sleep without feeling like choking.” This child was literally keeping her tongue from falling back into her airway with her thumb.
can fall back into the airway while sleeping. As a result they sleep only partially reclined. I once studied a patient who insisted on sucking their thumb at night, well into their middle school years, “because it’s the only way I can sleep without feeling like choking.” This child was literally keeping her tongue from falling back into her airway with her thumb.
With regards to speech, the child may have developed the use of a “w” sound to prononce “L” or “R,” since they are unable to contact their palate with their tongue. Similarly, their “sh” and “th” sounds won’t sound quite like it should, and the child may remain shy or self-conscious about speaking differently.
So if the body has to compensate for the tongue, what’s the harm in that?
Compensations are not a good thing. Compensations put too much stress on muscles that were not designed to do what the tongue does, and lead to adverse patterns in growth and 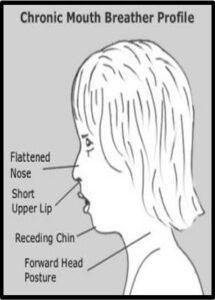 development. When a baby compensates during feeding, they must overuse the lip and cheek muscles to suck. They often get tired during feeds, get blisters on their lips, and swallow a lot of air, causing painful gas, reflux symptoms, and persistence of an immature swallow pattern. Over time, this sucking pattern puts an inward pressure on the palate, causing narrowing of the palate and nasal cavity. As the bones of the face are more narrowed, problems such as chronic congestion and mouth breathing can ensue, which in turn can lead to inflamed tonsils, narrow airway, frequent ear infections, and proneness to allergies.
development. When a baby compensates during feeding, they must overuse the lip and cheek muscles to suck. They often get tired during feeds, get blisters on their lips, and swallow a lot of air, causing painful gas, reflux symptoms, and persistence of an immature swallow pattern. Over time, this sucking pattern puts an inward pressure on the palate, causing narrowing of the palate and nasal cavity. As the bones of the face are more narrowed, problems such as chronic congestion and mouth breathing can ensue, which in turn can lead to inflamed tonsils, narrow airway, frequent ear infections, and proneness to allergies.
In adulthood, these same patients have often developed a permanent forward head posture, which uses gravity to bring the jaw forward, in order to open up the airway while simply at rest. This puts strain on the neck, spine, and shoulders, possibly leading to chronic pain, headaches, and stress on the body. Many of these same adults inevitably also suffer from sleep apnea as well, as the body continually must find ways to work around the obstruction of the tongue and the narrowing of the airway to gain more oxygen.
Only therapy can help eliminate these compensations, and the earlier it starts, the better.
Plenty of patients are misdiagnosed as having a restrictive tongue tie, and therapists are often able to assess whether it is a true restriction or more complex in scope.
Properly trained feeding and speech therapists are well-versed in the mechanics of oral muscle movement while functioning. They are able to tell, while the child is feeding or speaking, if the tongue movement is truly restricted during function, or if the problem is caused by something else that would require assessment by an appropriate medical professional. (Examples of conditions that mimic tongue tie restriction could be low muscle tone, atypical neurological patterns, or laryngomalacia).
But in a significant number of these cases, therapy alone can solve the problem! Certain conditions like muscle tension, womb positioning, or torticollis create feeding difficulties and affect tongue elevation. Plenty of patients that I have sent for therapy first never end up needing the tongue tie release. This is always a win for your child, because the uncomfortable stretching required for wound healing after the tongue tie release can be avoided.
The situation is equivalent to a severely arthritic knee needing surgery. Physical rehabilitation is always required in order to correct function of the knee and leg as a whole. Therapy is arguably more important than the surgery itself. The tongue is not just an individual entity; it’s a large muscle that is connected to tissues in the head and neck which are in turn connected to the rest of the body! Proper development starts with proper function, early on in life.
Do you want to schedule a consult to discuss a tongue tie? Call us anytime if you’d like more information! 337-981-9242 x1
Website | Facebook | Instagram | Twitter
Dr. Anita Gouri, a pediatric dentist, has been practicing in Lafayette for 10 years and is the  owner of Lafayette Pediatric Dentistry. She graduated from LSU School of Dentistry in 2006, receiving honors including Outstanding Achievement in Pediatric Dentistry, Honors in Research, and the Carl A. Baldridge Academic Scholarship. She completed her residency in pediatric dentistry at Children’s National Medical Center in Washington DC in 2008 and became a board certified diplomate of the American Board of Pediatric Dentistry in 2009. In 2010, her research on dental pain assessment was published in Pediatric Dentistry. She also has specialized training in treating babies and children who have tongue and lip ties. She is a member of the Academy of Laser Dentistry, American Academy of Pediatric Dentistry, the Louisiana Dental Association, the Southwestern Society of Pediatric Dentistry, American Dental Association, as well as the C. Edmund Kells and Omicron Kappa Upsilon Dental Honor Societies. Dr. Gouri, her husband, and their two children enjoy travel, Saints football, good food and good friends.
owner of Lafayette Pediatric Dentistry. She graduated from LSU School of Dentistry in 2006, receiving honors including Outstanding Achievement in Pediatric Dentistry, Honors in Research, and the Carl A. Baldridge Academic Scholarship. She completed her residency in pediatric dentistry at Children’s National Medical Center in Washington DC in 2008 and became a board certified diplomate of the American Board of Pediatric Dentistry in 2009. In 2010, her research on dental pain assessment was published in Pediatric Dentistry. She also has specialized training in treating babies and children who have tongue and lip ties. She is a member of the Academy of Laser Dentistry, American Academy of Pediatric Dentistry, the Louisiana Dental Association, the Southwestern Society of Pediatric Dentistry, American Dental Association, as well as the C. Edmund Kells and Omicron Kappa Upsilon Dental Honor Societies. Dr. Gouri, her husband, and their two children enjoy travel, Saints football, good food and good friends.